This is a topic that keeps coming up for me, both in my private and professional life, so I thought now is a great time to write this article on irritable bowel syndrome (IBS) and the low FODMAP diet. Personally, although I do not have IBS, one of my household members goes, which means we often cook using low-FODMAP foods at home. Read on to find out a bit more on IBS as well as on nutrition therapies for reducing its symptoms, including the low FODMAP diet.

What is irritable bowel syndrome?
Irritable bowel syndrome (IBS) is a diagnosis usually given for a collection of gastrointestinal symptoms. These vary from one person to another, but usually include abdominal pain/discomfort, bloating, and constipation and/or diarrhea. Some other common issues faced by those with IBS include lethargy, nausea, backache and bladder issues. IBS is a very common problem, with a global prevalence of 7-21%.
There are three primary subtypes of IBS, classified as diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), and both diarrhea and constipation (IBS-M). Although medical treatments exist, IBS symptoms are usually triggered by certain foods, which is why IBS is often managed with dietary modifications.
What are the nutritional recommendations for IBS patients?
First and foremost, it’s important to remember that if you’re experiencing persistent gastrointestinal symptoms you should consult your doctor. Your doctor will most likely ask about your symptoms and may also do some tests to rule out other issues, like celiac disease and inflammatory bowel disease. Once you’ve received a diagnosis of IBS, there are several things you could change in your diet to manage your symptoms:
Alcohol
Many individuals with IBS find that their symptoms get worse when they drink alcohol. If you notice that alcohol triggers your symptoms, avoiding or reducing your intake may help.
Fatty foods

It seems that individuals with IBS may have increased sensitivity to fatty foods, which can lead to symptoms like excessive fullness, bloating, and nausea. There is some evidence that fat also overstimulates a reflex called the gastrocolic reflex in individuals with IBS, which causes the colon to become overly motile (it starts moving things along too quickly), leading to diarrhea and pain. So, avoiding fried and processed foods may relieve symptoms, especially meal-related abdominal pain.
Spicy food
Spicy food often contributes to symptoms, so if you suspect this is the case, you can do a trial restriction by avoiding spicy foods. If symptoms get better, you will know to continue avoiding these foods in the future.
Dairy

Many individuals with IBS may also have lactose intolerance. If possible, it’s best to have this tested by your doctor. If this isn’t possible, you can try to cut lactose-containing foods (i.e. dairy) out of your diet as a trial to see if symptoms get better. However, keep in mind that cutting out dairy may result in low calcium intake, so it’s important to consider other sources of calcium and/or to discuss this with your doctor or dietitian. It is also possible to continue eating dairy in the form of lactose-free products, or to take a lactase pill before dairy-containing meals (see tips below).
Fluid
It may be helpful to gradually increase fluid intake to a total of 1.5 to 3 litres per day, especially for those with constipation-predominant IBS. Increased fluid intake can help increase your ability to pass stool.
Peppermint oil
There is some evidence that peppermint oil capsules (560-900 mg per day in divided doses) can help relieve IBS symptoms. However, keep in mind that these can get costly because you have to take them continuously for the effects to occur. They also cause heartburn for some people. However, if you’re looking for a “quick fix”, this may be a good option.
Elimination diets: the low FODMAP diet
The recommendations mentioned above are considered a first line approach for nutritional therapy for IBS. If these options fail, is it recommended to move on to the low FODMAP diet. The low FODMAP diet is an elimination diet, in which certain foods are eliminated and then slowly reintroduced while symptoms are carefully monitored. By the end of the process, you should be left with a personalized diet that excludes the foods that trigger your symptoms.
What are FODMAPs?
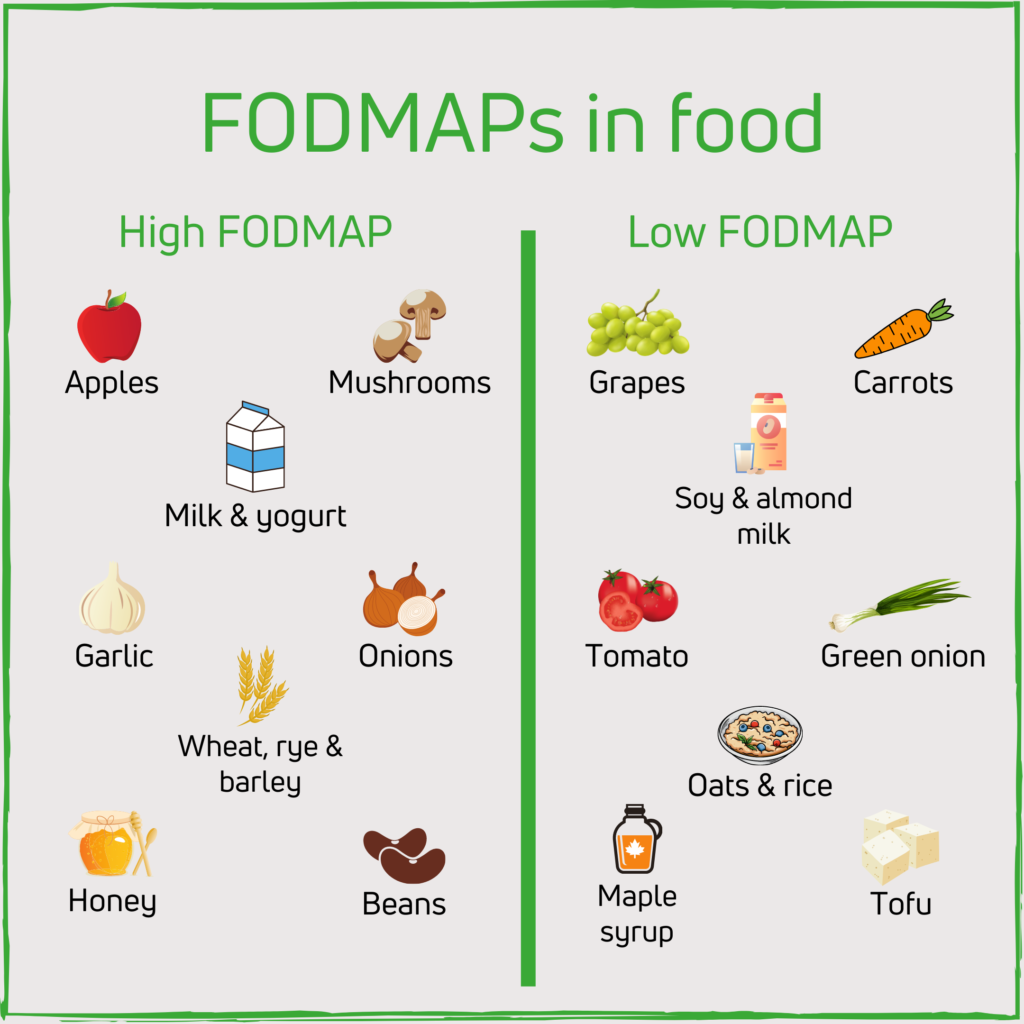
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. This may seem like a mouthful, but basically all of these are types of sugar molecules. These sugars are not well digested and absorbed by our small intestine, which means they attract water into the digestive system (which could cause diarrhea). Once they pass into the large intestine undigested, these sugars get fermented by our gut bacteria. This fermentation process produces gas, leading to bloating.
FODMAPs are found in a wide range of foods and cause few issues for those without IBS. However, it seems that people with IBS have a sensitive gut, so bloating can cause exaggerated feelings of pain and/or discomfort, which is the hallmark symptom of IBS. Therefore, avoiding certain FODMAPs can be a helpful way to manage IBS symptoms. In fact, studies show that a low FODMAP diet can help reduce symptoms like abdominal pain/discomfort, bloating, diarrhea, and constipation.
The three steps of a low FODMAP diet
Elimination
So how do you get started on a low FODMAP diet? The first step is elimination. For 2-6 weeks, you need to avoid high FODMAP foods. This can be difficult, but luckily there are many lists and even smartphone applications that can help you learn which foods to avoid (see More resources below).
Reintroduction
Once elimination is done, you can start reintroducing FODMAPs slowly back into your diet, usually over 8-12 weeks. It’s best to reintroduce one FODMAP food group at a time over three days. Once you do, monitor your symptoms to understand how much of that food you’re able to tolerate.
Personalization
Over the long term, you will start learning which foods you are able to tolerate and in what amounts. It’s important to keep going with reintroduction and personalization of your diet in order to bring back as many foods as you are able to tolerate. At the end of the day, it’s important to have variety in your diet and to not avoid foods unless you really have to.
Some low FODMAP swaps and tips
To use instead of onion
- Green onion: green section only
- Chives: dry or fresh
- Leeks: green section only, up to ⅔ cup
To use instead of garlic
- Chives: dry or fresh
- Garlic oil
Other flavourings that are low FODMAP
A low FODMAP diet doesn’t have to be bland. Low FODMAP flavourings include ginger, most spices and herbs, lemon/lime, and stocks that are not made with onion/garlic.
Enzymes
Enzymes are molecules that can help you digest things you normally would not be able to digest. We naturally have different kinds of enzymes in our digestive system, but we are missing those that digest FODMAPs. Conveniently, you can buy some of these enzymes in pill form! Specifically, here are two kinds that I have found can be helpful:
- Lactase: if lactose intolerance is contributing to your IBS but you still want to eat dairy products, it may be worth it to invest in some lactase. Lactase is the enzyme that breaks down lactose, the milk sugar that makes you feel sick. You can buy it in pill form and take it with dairy, or in liquid form that you add directly to food. Another option is buying lactose-free products, which have become more popular in recent years and can be found at most supermarkets.
- Alpha-galactosidase: this is the enzyme in Beano, but it can be found in many generic brands as well. This enzyme can break down some of the undigestible sugars found in legumes (e.g. beans, chickpeas). If you take it with your meals, it may reduce the gas and bloating you experience.
Low FODMAP recipes
More resources
For a complete guide to the low FODMAP diet, as well as for a list of high FODMAP and low FODMAP foods, I highly suggest you take a look at Monash University’s website and/or smartphone application. Monash University is the institution responsible for the development of the low FODMAP diet and has excellent resources for the public and for healthcare professionals.
There are also dietitians who specialize in IBS who could be a valuable source of information and support. Following this diet can be challenging and overwhelming, so if you are able to see a dietitian, I recommend you do so. If you live in Canada, you could use Dietitians of Canada’s Find a Dietitian webform to look for a dietitian that specializes in this field.
References
- British Dietetic Association. Irritable Bowel Syndrome and Diet : Food Fact Sheet. Retrieved from https://www.bda.uk.com/resource/irritable-bowel-syndrome-diet.html.
- Dietitians of Canada. Gastrointestinal System – Irritable Bowel Syndrome Practice Guidance Toolkit. In: Practice-based Evidence in Nutrition® [PEN]. 2018 July 24 [cited 2020 July 30]. Available from: http://www.pennutrition.com.
- Dietitians of Canada. Irritable Bowel Syndrome Summary of Recommendations and Evidence. In: Practice-based Evidence in Nutrition® [PEN]. 2018 July 24 [cited 2020 July 30]. Available from: http://www.pennutrition.com.
- McKenzie, Y. A. et al. (2016). British Dietetic Association systematic review and evidence- based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). Journal of Human Nutrition and Dietetics, 29, 549-575.
- Monash University. FODMAPs and Irritable Bowel Syndrome. Retrieved from https://www.monashfodmap.com/about-fodmap-and-ibs/.

One Reply to “Irritable Bowel Syndrome and the Low FODMAP Diet”
Comments are closed.